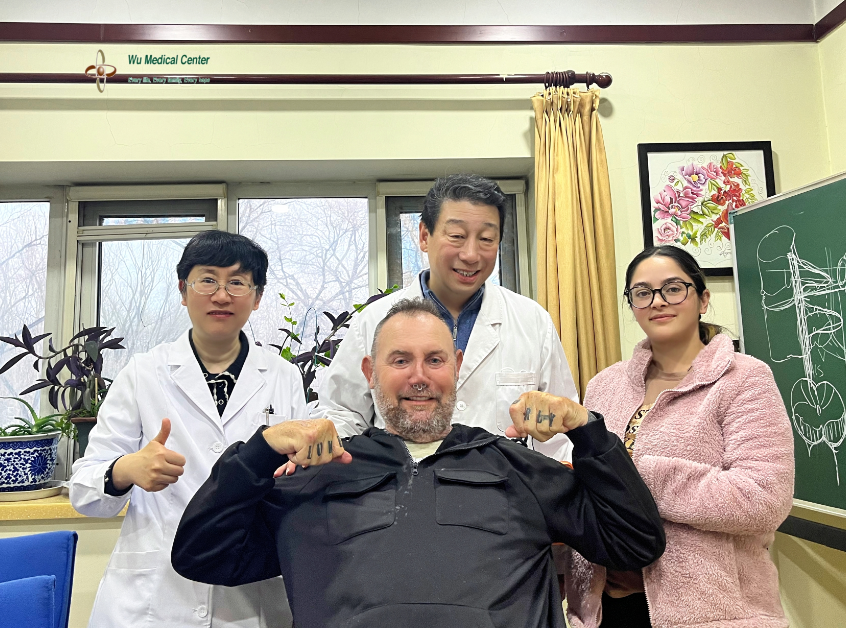
Todd Clifford Johnston-Motor Neuron Disease - Primary Lateral Sclerosis; Type 2 Diabetes Mellitus-(Australian)
 Patient's Name: Todd Clifford Johnston
Patient's Name: Todd Clifford Johnston
Gender: Male
Age: 58 years old
Nationality: Australian
Diagnosis: Motor Neuron Disease - Primary Lateral Sclerosis; Type 2 Diabetes Mellitus
Condition Upon Admission:
The patient was admitted to the hospital with a diagnosis of Motor Neuron Disease - Primary Lateral Sclerosis, mainly due to "progressive dysarthria accompanied by limb weakness for 13 years, with exacerbation over the past 2 years". He was unable to speak and presented with dysarthria, limb weakness, and stiff, slow movements. He could not get up or walk independently and had almost no self-care ability. He also exhibited an anxious mental state. The patient had a history of Type 2 Diabetes Mellitus and asthma.
Physical Examination on Admission:
The patient’s pulse was 92 beats per minute, respiratory rate was 20 breaths per minute, blood pressure was 121/86 mmHg, and blood oxygen saturation was 93–94%. He had a normal build and satisfactory nutritional status. There was mild cyanosis of the lips, and slight congestion and swelling of the pharynx. Respiratory excursion was basically normal; breath sounds over the bilateral lower lungs were diminished, without obvious moist or dry rales. Heart sounds were normal with a regular rhythm, and no murmurs were heard over each valvular area of the heart. The abdomen was flat and soft, with no hepatosplenomegaly (liver and spleen not palpable below the costal margins). There was edema of the feet in both lower extremities.
Neurological Examination:
The patient was conscious, with slightly poor mental status and an anxious expression. He was basically unable to produce speech sounds. His eye movements were flexible in all directions. His tongue protruded centrally, with slow lingual muscle movements and no obvious tongue atrophy. He had weak cheek puffing strength, but his masticatory strength was fair. The elevation of his bilateral soft palates was strong, and the uvula was positioned centrally. His neck rotation and shoulder shrugging strength were adequate, with the muscle strength of bilateral sternocleidomastoid muscles graded as Grade 4. The muscle strength of biceps brachii in both upper limbs was Grade 4-, and that of triceps brachii was Grade 3-. The strength of wrist dorsiflexion, palmar flexion, and grip strength of both hands was Grade 3. The muscle strength of both lower limbs was Grade 3-. When lying supine, he could only maintain hip and knee flexion to lift his lower limbs off the bed for 5 seconds. The abduction of both lower limbs was significantly limited, with a maximum abduction angle of only about 10° bilaterally, accompanied by obvious tremors and inability to resist external force. He was unable to stand up or walk independently and required significant assistance. With the support of a walker, he could walk extremely slowly for approximately 15 meters, presenting with a narrow gait base and uncoordinated posture. His limb muscle tone was increased, and muscle atrophy was observed in all limbs, which was more pronounced in the hands. His limb sensation was normal. Tendon reflexes of all limbs were hyperactive, and pathological reflexes of all limbs were positive. For the finger-opposition test, he could only complete the movement with his index fingers. His rapid alternating hand movements were slow, with the right side being notably impaired. He was unable to perform the heel-knee-tibia test for both legs due to muscle weakness. Meningeal irritation signs were negative.
Treatment Process:
The patient was clearly diagnosed with Motor Neuron Disease - Primary Lateral Sclerosis and Type 2 Diabetes Mellitus upon admission. During hospitalization, he was administered neural stem cell therapy to repair motor nerve damage, along with mesenchymal stem cell therapy to provide neurotrophic, endocrine and immune support. Adjuvant CAST therapy was given with medications including edaravone, riluzole, neurotrophic factors and reduced glutathione. Comprehensive rehabilitation therapy was also implemented in combination with the above treatments.
Post-Treatment Condition:
The patient's motor function improved. He was able to make monosyllabic sounds, which were clearer and louder than before. His limb motor function was enhanced with increased muscle strength: the muscle strength of the biceps brachii in both upper limbs reached Grade 5, and that of the triceps brachii was Grade 4-, with both arms able to resist considerable external resistance. The strength of wrist dorsiflexion, palmar flexion and grip strength of both hands was Grade 4. The muscle strength of both lower limbs was Grade 4-. His movement flexibility was significantly improved. With the support of a walker, he could walk approximately 60 meters, with a wider and more stable gait base than before. The range of motion of his limbs increased; the abduction angle of both lower limbs reached about 20 degrees, and the tremor was significantly relieved. He could now complete the finger-opposition test with his middle fingers, and his performance on the rapid alternating hand movements test was much better than previously. His cardiopulmonary function was improved compared with that upon admission, with a heart rate of approximately 70–80 beats per minute and blood oxygen saturation of 94–96%.